
Microneedling Contraindications: Key Safety Factors
Understanding Microneedling Contraindications for Safer Treatments
Microneedling rejuvenates skin, but isn't suitable for everyone. Certain conditions, or microneedling contraindications, can make the procedure risky or ineffective. This listicle explores seven key microneedling contraindications practitioners and clients should know. Understanding these contraindications allows for safer treatments and better outcomes.
This guide helps you:
Identify conditions unsuitable for microneedling
Minimize potential risks and side effects
Make informed decisions about skincare treatments
Ensure client safety during microneedling procedures
Whether you're an aesthetician or exploring microneedling for yourself, this information is crucial. Safe treatment begins with understanding who shouldn't undergo microneedling. We'll cover active acne, keloids, blood clotting disorders, pregnancy, autoimmune conditions, rosacea, and recent cosmetic procedures, explaining why each presents a contraindication for microneedling.
1. Active Acne Breakouts and Infections
Microneedling, a popular treatment for skin rejuvenation, involves creating microscopic punctures in the skin to stimulate collagen and elastin production. While generally safe and effective, microneedling has specific contraindications that must be carefully considered. One of the most important is the presence of active acne breakouts and infections. Performing microneedling on skin with active acne, bacterial, fungal, or viral infections can have adverse consequences.

The tiny needles used in microneedling create channels into the skin. If these channels are created on or near active breakouts, the needles can inadvertently spread the infection. This can push bacteria and other infectious material deeper into the skin or transfer it to previously unaffected areas, exacerbating the existing condition and potentially creating new infection sites.
Understanding the Risks
Imagine using a tiny needle to prick an infected pimple and then using that same needle to prick healthy skin. This illustrates how microneedling on infected skin can spread pathogens. This can lead to more widespread breakouts, delayed healing, and even scarring. It's crucial to understand that this applies not only to acne but also to other skin infections like impetigo, herpes simplex, and fungal infections. For clients with acne scarring, waiting for active breakouts to clear is crucial before beginning microneedling treatments. Learn more about...
Examples of Complications
Several scenarios highlight the risks of microneedling over active infections:
Cystic Acne: A patient with cystic acne undergoes microneedling and subsequently develops widespread pustular breakouts across the treated area.
Herpes Simplex Reactivation: Microneedling can trigger a herpes outbreak, particularly in individuals with a history of the virus. This can lead to a painful and extensive facial rash.
Impetigo Spread: Microneedling over a patch of impetigo can cause the highly contagious bacterial infection to spread rapidly across the face.
Essential Precautions and Tips
To ensure client safety and successful microneedling outcomes, consider these crucial steps:
Thorough Skin Assessment: Before every microneedling session, conduct a meticulous skin assessment to identify any active breakouts or infections. This is paramount for preventing complications.
Resolution of Breakouts: Postpone microneedling until all active breakouts have completely resolved. Patience is key to achieving optimal results and minimizing risks.
Prophylactic Measures: For clients with a history of herpes simplex outbreaks, antiviral prophylaxis is often recommended before and after microneedling to prevent reactivation.
Topical Antibiotics: Minor localized infections might be addressed with topical antibiotics before considering microneedling. Consult with a dermatologist to determine the appropriate course of action.
Addressing active acne breakouts and infections before microneedling is a non-negotiable aspect of responsible practice. Prioritizing skin health and patient safety is essential to delivering effective and complication-free treatments. This careful approach underscores the importance of understanding microneedling contraindications for successful outcomes.
2. Keloid and Hypertrophic Scar Formation History
Microneedling, while effective for skin rejuvenation, isn't suitable for everyone. A crucial contraindication is a history of keloid or hypertrophic scarring. These individuals have an increased risk of abnormal wound healing responses. Microneedling creates controlled micro-injuries, which can trigger excessive collagen production in susceptible individuals. This can lead to raised, thick scars extending beyond the original treatment area. Understanding this risk is paramount for safe and effective microneedling practices.
The tiny punctures created during microneedling stimulate collagen and elastin production. However, for those prone to keloids or hypertrophic scars, this process can go awry. Instead of smooth, rejuvenated skin, they may develop unsightly raised scars. This is because their bodies react to the micro-injuries by overproducing collagen, forming a fibrous, elevated scar.
Understanding the Risks
Keloids and hypertrophic scars, while benign, can be aesthetically displeasing and sometimes itchy or painful. They can occur anywhere on the body but are more common on the chest, back, shoulders, and earlobes. For individuals with a predisposition to these types of scars, even minor skin trauma, like microneedling, can trigger their formation.
Examples of Complications
Several scenarios highlight the risks:
Keloid After Ear Piercing: A patient with a history of keloid formation from an ear piercing developed raised scars after facial microneedling.
Family History of Keloids: An individual with a family history of keloids experienced hypertrophic scarring after acne scar treatment with microneedling.
Chest Microneedling: Chest microneedling resulted in keloid formation requiring corticosteroid injections for treatment.
Essential Precautions and Tips
To mitigate risks and ensure client safety, follow these steps:
Thorough History Assessment: Conduct a detailed personal and family history assessment regarding keloid or hypertrophic scar formation before any microneedling procedure.
Patch Testing: Consider a patch test in an inconspicuous area before treating larger areas. This helps assess the skin's response to microneedling.
Shorter Needle Lengths: If microneedling is deemed necessary, use shorter needle lengths (0.25-0.5mm) to minimize the risk of excessive collagen stimulation.
Keloid Treatment Options: Have keloid treatment options readily available should they occur, including silicone sheets, corticosteroid injections, or laser therapy.
Assessing a client's history of keloid and hypertrophic scar formation is vital when considering microneedling. This careful approach, combined with appropriate precautions, is essential for responsible and successful microneedling treatments, minimizing the risk of undesirable outcomes. This understanding of microneedling contraindications helps ensure client satisfaction and safety.
3. Blood Clotting Disorders and Anticoagulant Medications
Microneedling, while generally safe, involves creating numerous micro-punctures in the skin. This makes it crucial to consider pre-existing conditions that could affect the body’s natural clotting process. Individuals with blood clotting disorders or those taking anticoagulant medications are at increased risk for complications during and after microneedling. These complications can include prolonged bleeding, excessive bruising, and impaired wound healing. Understanding these risks is a critical aspect of responsible microneedling practice.
The tiny punctures created during microneedling typically heal quickly in healthy individuals. However, for those with compromised clotting abilities, these micro-injuries can pose a greater challenge. Conditions like hemophilia, thrombocytopenia, and von Willebrand disease can significantly impact the body's ability to form blood clots, increasing the risk of prolonged bleeding at the puncture sites. Similarly, anticoagulant medications, commonly known as blood thinners, can interfere with the clotting cascade and increase bleeding risk.
Understanding the Risks
The risks associated with microneedling for individuals with clotting disorders or taking anticoagulants are not trivial. Prolonged bleeding can lead to hematoma formation, which is a localized collection of blood outside the blood vessels. Excessive bruising can also occur, lasting significantly longer than usual and potentially causing discomfort and cosmetic concerns. Impaired wound healing can delay the skin's recovery process and increase the risk of infection or scarring. Addressing these microneedling contraindications is vital.
Examples of Complications
Several scenarios demonstrate the potential complications:
Warfarin Use: A patient on warfarin for atrial fibrillation underwent microneedling and experienced significant facial bruising that lasted for three weeks.
Hemophilia: An individual with hemophilia underwent microneedling and experienced persistent bleeding from the treatment sites, requiring medical intervention to control the bleeding.
Fish Oil Supplements: A patient taking high-dose fish oil supplements, which can have blood-thinning effects, underwent microneedling and experienced delayed healing and increased inflammation.
Essential Precautions and Tips
To ensure patient safety and mitigate potential complications, consider these essential precautions:
Detailed Medical History: Obtain a thorough medical history, including any bleeding disorders, current medications, and supplements. Specifically inquire about anticoagulants, antiplatelet medications, and even over-the-counter NSAIDs like ibuprofen.
Physician Consultation: If a client has a bleeding disorder or takes anticoagulants, consult with their prescribing physician before proceeding with microneedling. This collaborative approach is crucial for determining the best course of action.
Temporary Discontinuation: In some cases, temporary discontinuation of non-essential blood thinners may be considered under the guidance of the prescribing physician. This should never be done without medical supervision.
Hemostatic Agents: Have hemostatic agents readily available during the microneedling procedure to control any excessive bleeding that may occur.
By carefully considering these microneedling contraindications and implementing appropriate precautions, practitioners can minimize risks and ensure the safety and well-being of their clients. A proactive approach to patient assessment and communication is crucial for successful and complication-free microneedling treatments.
4. Pregnancy and Breastfeeding
Microneedling, while effective for skin rejuvenation, is contraindicated during pregnancy and breastfeeding. This is primarily due to the significant hormonal shifts during these periods, which influence skin sensitivity, healing processes, and the potential for increased absorption of topical products. Furthermore, the general principle of avoiding elective cosmetic procedures during pregnancy and breastfeeding applies to microneedling. Hormonal fluctuations can also unpredictably affect pigmentation, leading to uneven skin tone.

The skin's reactivity is heightened during pregnancy and breastfeeding. This increased sensitivity can make the skin more susceptible to irritation and inflammation following microneedling. The healing process may also be altered, potentially leading to prolonged redness, swelling, or even scarring. Additionally, certain topical products used in conjunction with microneedling may be absorbed into the bloodstream, posing potential risks to the developing fetus or nursing infant.
Understanding the Risks
Hormonal changes during pregnancy can lead to conditions like melasma (dark patches on the skin). Microneedling during this time can exacerbate melasma or trigger its development, leading to unwanted pigmentation changes that are difficult to reverse. The altered healing responses during pregnancy and breastfeeding also increase the risk of complications like prolonged inflammation or infection. Moreover, the safety of many topical products used with microneedling has not been established for pregnant or breastfeeding women.
Examples of Complications
Consider these scenarios illustrating potential complications:
Melasma Development: A pregnant patient undergoes microneedling and develops persistent melasma, which remains even after delivery.
Skin Irritation: A breastfeeding mother experiences severe skin irritation and delayed healing after microneedling, impacting her ability to nurse comfortably.
Uneven Pigmentation: A post-partum patient has uneven pigmentation following microneedling that requires months to resolve.
Essential Precautions and Tips
To ensure client safety and avoid complications, follow these guidelines:
Screening for Pregnancy: Screen all female patients of childbearing age for pregnancy before microneedling. This is a critical step in risk mitigation.
Postponing Treatment: Recommend waiting until after breastfeeding is complete before undergoing microneedling. This ensures hormonal stability and minimizes potential risks to the infant.
Gentle Skincare: Encourage gentle skincare routines during pregnancy and breastfeeding. Focus on hydration and sun protection rather than invasive procedures.
Post-Weaning Treatments: Schedule microneedling treatments for 3-6 months post-weaning for optimal results and minimal risk of complications.
Recognizing pregnancy and breastfeeding as microneedling contraindications is crucial for responsible practice. Prioritizing client safety and well-being during these sensitive periods demonstrates a commitment to providing ethical and effective care. By understanding these contraindications, practitioners can guide clients towards appropriate skincare choices and help them achieve their aesthetic goals safely.
5. Autoimmune and Immunocompromised Conditions
Microneedling, while generally safe, presents specific challenges for individuals with autoimmune or immunocompromised conditions. These conditions, ranging from lupus and rheumatoid arthritis to HIV and cancer treatments, alter the body's immune response. This can significantly impact how the skin reacts to microneedling, affecting healing, increasing infection risk, and potentially triggering unpredictable inflammatory reactions.
The controlled micro-injuries induced by microneedling are designed to stimulate collagen production. However, in individuals with compromised immune systems, this process can be disrupted. Their bodies may struggle to heal efficiently, increasing the risk of prolonged inflammation, infection, and even scarring. Furthermore, the inflammatory response itself can exacerbate underlying autoimmune conditions, leading to flare-ups and other complications.
Understanding the Risks
Microneedling creates microscopic wounds, which are normally part of the healing and rejuvenation process. For someone with a healthy immune system, this is beneficial. However, for individuals with weakened immunity, these micro-wounds can become entry points for infections. Their bodies may not be able to effectively fight off bacteria or other pathogens, leading to complications. Moreover, the treatment itself can trigger or worsen existing autoimmune conditions, causing a cascade of unwanted reactions.
Examples of Complications
Several scenarios highlight the potential risks:
Lupus Flare: A patient with lupus undergoes microneedling and experiences a severe facial rash and joint pain flare-up following the treatment.
Infection Post-Chemotherapy: A patient undergoing chemotherapy develops a persistent infection at the microneedling site, requiring hospitalization.
Delayed Healing and Scarring: An organ transplant recipient experiences significantly delayed healing and subsequent scarring after microneedling due to their immunosuppressed state.
Essential Precautions and Tips
Given the heightened risks, specific precautions are essential when considering microneedling for individuals with autoimmune or immunocompromised conditions:
Medical Clearance: Always require medical clearance from the patient's treating physician before proceeding with microneedling. This ensures the treatment is safe and appropriate given their specific condition and current health status.
Timing and Remission: If possible, consider timing microneedling treatments during periods of disease remission to minimize the risk of complications.
Conservative Approach: Use conservative treatment parameters, including shallower needle depths and lower treatment frequency, to reduce the intensity of the skin's response.
Strict Sterile Technique: Maintain impeccable sterile technique throughout the procedure and emphasize meticulous post-care protocols to minimize infection risk.
For patients with autoimmune and immunocompromised conditions, microneedling requires a cautious and individualized approach. Prioritizing patient safety and open communication with their healthcare providers are crucial for mitigating risks and ensuring the best possible outcomes. Understanding these microneedling contraindications is fundamental to responsible practice.
6. Rosacea and Sensitive Skin Conditions
Microneedling, while beneficial for many, is not suitable for all skin types. Specifically, individuals with rosacea, eczema, dermatitis, and other inflammatory skin conditions should proceed with extreme caution, if at all. These conditions often involve a compromised skin barrier, heightened sensitivity, and increased reactivity. Microneedling can exacerbate these issues, triggering inflammatory flares, worsening existing conditions, and causing prolonged irritation.

The controlled micro-injuries induced by microneedling are intended to stimulate collagen production. However, for sensitive skin, this can backfire. The process can intensify inflammation, leading to redness, burning, itching, and the formation of papules or pustules. In some cases, these reactions can persist for weeks or even months, significantly impacting a person's quality of life. Understanding the potential risks is crucial for both practitioners and clients considering microneedling.
Understanding the Risks
The skin barrier's primary function is to protect against external irritants and pathogens. Conditions like rosacea and eczema compromise this barrier, making the skin more vulnerable to inflammation. Microneedling, by its very nature, disrupts this already fragile barrier, potentially triggering a cascade of inflammatory responses. This underscores the importance of careful consideration and thorough assessments before proceeding with microneedling for individuals with sensitive skin. For further information on microneedling and related skin conditions, learn more about....
Examples of Complications
Several cases illustrate the potential risks of microneedling on sensitive skin:
Rosacea Flare: A patient with rosacea underwent microneedling and experienced severe facial flushing and the development of papules that persisted for months.
Eczema Exacerbation: An individual with eczema developed contact dermatitis requiring steroid treatment after a microneedling session.
Persistent Irritation: A person with sensitive skin, not diagnosed with a specific condition, experienced prolonged erythema and a burning sensation following microneedling.
Essential Precautions and Tips
To minimize risks for clients with sensitive skin:
Thorough Skin Assessment: Use validated scales to assess skin type and sensitivity before considering microneedling.
Conservative Approach: Perform a patch test or treat a very small, inconspicuous area first to gauge the skin's reaction.
Minimal Needle Depth: If microneedling is deemed appropriate, use minimal needle depths (0.25mm or less).
Anti-Inflammatory Measures: Have appropriate anti-inflammatory treatments readily available to manage potential reactions.
Microneedling can be a powerful tool for skin rejuvenation, but it's not universally suitable. Recognizing contraindications like rosacea and sensitive skin is essential for responsible practice. Prioritizing client safety and managing expectations are crucial for achieving positive and complication-free outcomes.
7. Recent Cosmetic Procedures and Treatments
Microneedling, while effective for skin rejuvenation, isn't always compatible with other cosmetic procedures. Recent treatments like chemical peels, laser procedures, Botox, and dermal fillers can create contraindications for microneedling. This is due to increased skin sensitivity, ongoing healing processes, or potential interactions with injected materials. Carefully considering the timing and combination of treatments is crucial for client safety and optimal results.
The skin's condition after cosmetic procedures can make it more vulnerable to complications during microneedling. For instance, skin treated with a chemical peel is often thinner and more sensitive, making it prone to irritation or hyperpigmentation if microneedling is performed too soon. Similarly, areas recently injected with fillers might experience uneven results or nodule formation if disrupted by microneedling needles.
Understanding the Risks
Combining treatments without proper consideration can lead to adverse reactions. Microneedling too soon after a laser treatment can exacerbate inflammation and potentially cause scarring. Similarly, introducing microneedling before Botox has fully settled can interfere with its distribution and effectiveness. Understanding these interactions is essential for providing safe and effective treatment plans.
The following infographic visualizes recommended waiting periods between common cosmetic procedures and microneedling. These safety intervals help minimize the risk of complications and ensure the skin has adequately recovered.
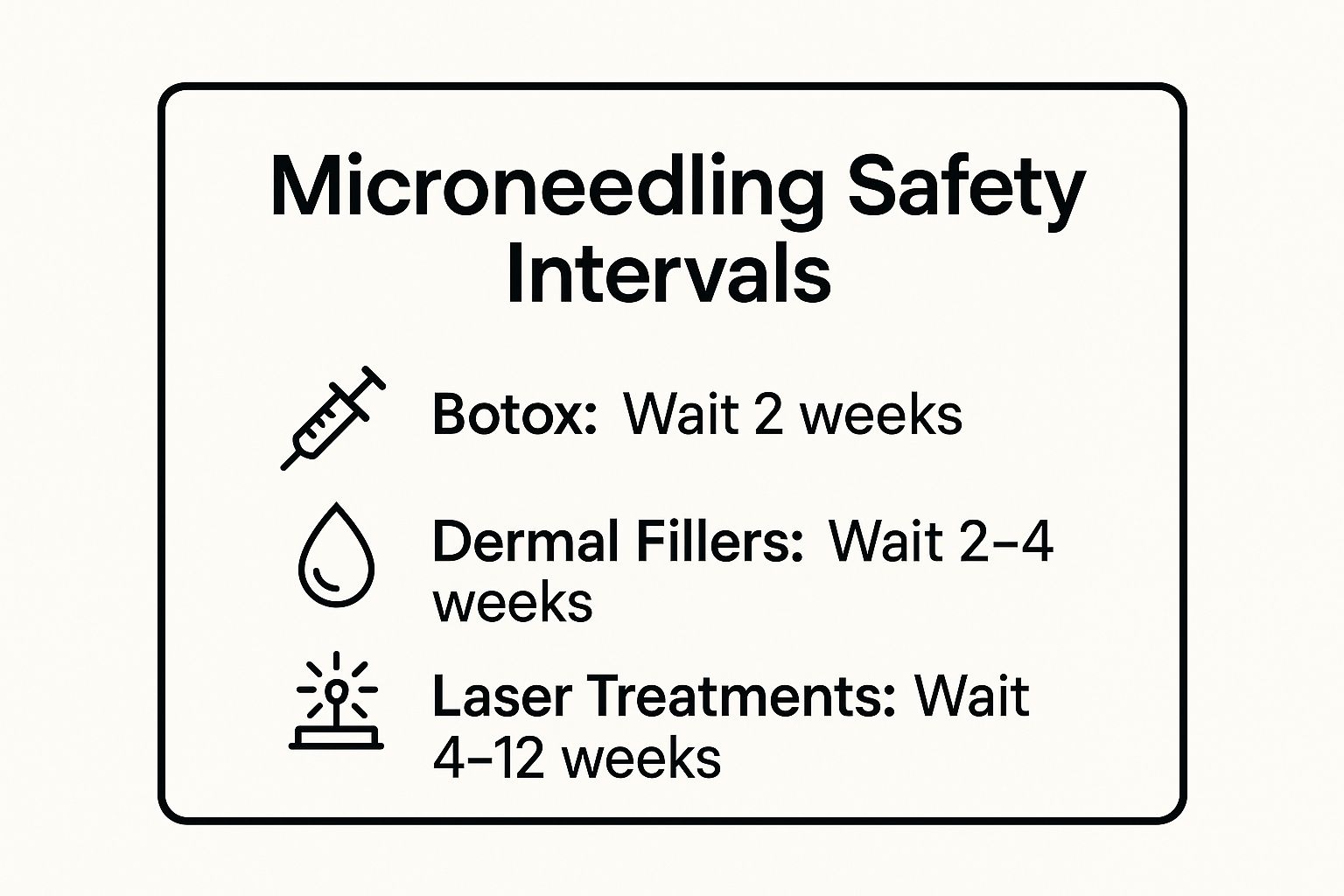
As the infographic highlights, procedures like Botox require a shorter waiting period of two weeks, while dermal fillers and laser treatments necessitate longer intervals of 2-4 weeks and 4-12 weeks, respectively. Adhering to these guidelines helps minimize potential complications and maximize treatment efficacy.
Examples of Complications
Several scenarios illustrate the risks of combining treatments prematurely:
Filler Migration: A patient who received hyaluronic acid fillers experienced nodule formation and uneven texture after undergoing microneedling too soon after the filler treatment.
Hyperpigmentation: A recent chemical peel recipient developed severe hyperpigmentation after microneedling due to the increased photosensitivity of the treated skin.
Scarring: A laser treatment patient experienced prolonged inflammation and scarring after premature microneedling, hindering the overall healing process.
Essential Precautions and Tips
To ensure client safety and successful outcomes when combining treatments, follow these crucial steps:
Detailed Records: Maintain meticulous treatment history records, noting dates, types of procedures, and product details.
Waiting Periods: Adhere to established waiting periods between procedures. This allows the skin to heal and reduces the risk of adverse reactions.
Collaboration: Coordinate with other treating practitioners to ensure consistent and safe treatment plans for clients undergoing multiple procedures.
Cumulative Effects: Consider the cumulative effects of multiple treatments on the skin’s barrier function and overall health.
Treatment Sequencing: Carefully plan the sequence and timing of procedures for optimal results. For example, microneedling might be scheduled after Botox has taken full effect but well before a planned laser treatment. Learn more about combining treatments effectively...
Understanding the interaction between microneedling and recent cosmetic procedures is paramount for practitioners. Prioritizing client safety and well-being through careful planning and adherence to established guidelines ensures effective and complication-free treatments. This comprehensive approach optimizes results and promotes overall skin health.
Microneedling Contraindications: 7 Key Factors Comparison
Condition / Factor Implementation Complexity Resource Requirements Expected Outcomes Ideal Use Cases Key Advantages Active Acne Breakouts and Infections High – contraindicated during active outbreaks Requires pre-treatment infection control, antiviral/antibiotic prophylaxis High risk of spreading infection and scarring Treatment postponed until clear skin Prevents worsening and systemic spread Keloid and Hypertrophic Scar History Moderate – careful needle length and test areas needed Patient history assessment, availability of scar treatments Risk of abnormal scar formation, permanent cosmetic issues Patients without known scar history or with mild scars Minimizes risk of raised scars Blood Clotting Disorders and Anticoagulants High – coordination with physicians essential Medical clearance, medication adjustments, hemostatic agents Possible prolonged bleeding, bruising, delayed healing Patients with normal clotting profile Ensures safer healing and reduces complications Pregnancy and Breastfeeding Low – generally contraindicated Pregnancy screening, alternative gentle treatments Unpredictable pigmentation and healing Non-pregnant, non-lactating patients Protects fetus/infant; avoids complications Autoimmune and Immunocompromised Conditions High – requires medical clearance and cautious approach Physician approval, sterile technique, possible prophylactic antibiotics Increased infection risk, delayed healing, unpredictable flares Patients in remission with stable conditions Limits disease flares and infection Rosacea and Sensitive Skin Conditions Moderate – requires patch testing and conservative parameters Skin assessment tools, anti-inflammatory treatments Possible inflammatory flares, prolonged irritation Mild or stable sensitive skin patients Reduces irritation and flare severity Recent Cosmetic Procedures and Treatments Moderate to High – timing and coordination critical Detailed treatment history, adherence to waiting periods Risk of filler displacement, hyperpigmentation, skin damage Patients with sufficient interval since last procedure Optimizes combined treatment safety
Prioritizing Safety and Efficacy in Your Microneedling Practice
This comprehensive guide has explored seven key microneedling contraindications, ranging from active acne and keloid scarring to pregnancy and autoimmune conditions. Understanding these contraindications is not merely a matter of professional due diligence; it's the foundation upon which safe and effective microneedling practices are built. By recognizing these potential risks, practitioners can make informed decisions, personalize treatment plans, and ultimately, prioritize client safety.
The Power of Informed Consent and Client Education
One of the most crucial takeaways from this article is the importance of informed consent. Clients need to be fully aware of the potential risks associated with microneedling, especially if they have any underlying conditions. Open communication and thorough consultations are essential for building trust and empowering clients to actively participate in their skincare journey. Providing detailed information about contraindications helps clients understand why certain treatments may not be suitable for them, fostering a collaborative approach to achieving their skincare goals.
Mastering Microneedling Contraindications for Optimal Results
Why is understanding microneedling contraindications so vital? Because it directly impacts treatment outcomes. Ignoring these contraindications can lead to adverse reactions, compromising both the client's health and the practitioner's reputation. By mastering this knowledge, practitioners can:
Minimize the risk of complications
Enhance treatment efficacy
Build client confidence and trust
Establish themselves as knowledgeable professionals
Beyond the Basics: Taking Your Microneedling Practice to the Next Level
This article has provided a foundation for understanding microneedling contraindications. However, ongoing learning is crucial in the ever-evolving field of aesthetics. Staying updated on the latest research, guidelines, and best practices is essential for providing the highest quality of care. Continuously expanding your knowledge will not only improve your skills but also demonstrate your commitment to client safety and optimal results.
This deep understanding of microneedling contraindications empowers you to offer personalized, effective treatments, leading to greater client satisfaction and ultimately, building a thriving practice centered around safety and positive outcomes. For personalized guidance and treatments tailored to your specific skin concerns, taking contraindications into careful account, visit Olive Skin Therapy. Olive Skin Therapy prioritizes client safety and provides expert consultations to determine the most suitable treatment approach, including assessing for any potential microneedling contraindications.
